Published 26 Sept 2025
Article by
5 min read
What is a Physical Therapy SOAP Note?
A physical therapy SOAP note is a method of documentation that follows a specific format to provide a way for therapists to record a patient’s progress and treatment plan in a clear and concise manner. This follows the SOAP—Subjective, Objective, Assessment, and Plan—method and is essential for communicating with other healthcare professionals and for legal purposes.
Importance of SOAP Notes in Physical Therapy
Physical Therapy (PT) is a critical part of rehabilitation for patients who have suffered from injuries, surgeries, or illnesses. PTs work with patients to help them regain their mobility, strength, and independence.
One of the most important tools that physical therapists use to document their patient’s progress is the SOAP note. Physical therapy SOAP notes present the following benefits, among others:
1. Consistency in Documentation and Recordkeeping
When a physical therapist uses a SOAP note template, they are ensuring that they document all the essential information in a standardized manner. This makes it easier for other healthcare professionals to read and understand the documentation, which can be essential in interdisciplinary care.
2. Better Patient Care
Using a SOAP note template can also help physical therapists to better track their patients’ progress. This way, they can create more personalized care programs and ensure better patient outcomes.
3. Legal Protection
Legally, physical therapists can demonstrate that they have provided appropriate patient care through SOAP note documentation. On the other hand, SOAP notes can serve as legal proof of a patient’s treatment and progress in the event of a lawsuit or insurance claim.
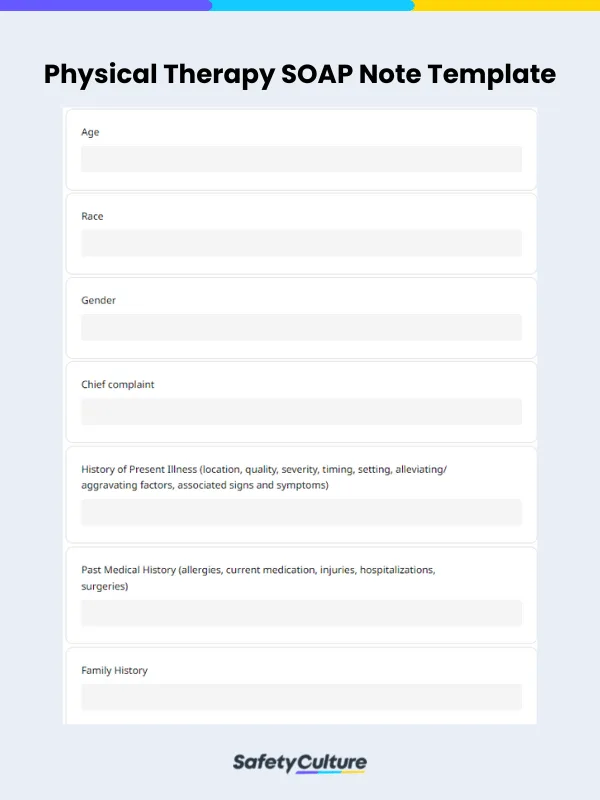
What to Include in a Physical Therapy SOAP Note
To ensure quality care to physical therapy patients, the following sections of a SOAP note for physical therapy must be included and contain accurate information:
Subjective Section
This section includes the patient’s description of their condition, symptoms, and any changes since their last appointment. It should be written in the patient’s own words and should include any relevant information about their medical history or current lifestyle.
Objective Section
This is where you indicate measurable data such as vital signs, range of motion, muscle strength, and any other physical measurements or observations that are relevant to the patient’s condition. This section should be based on objective, observable facts and should be as specific as possible. For example, instead of simply noting that the patient has pain in their knee, the therapist should document the location and severity of the pain, as well as any factors that exacerbate or alleviate the pain.
Assessment Section
To document the therapist’s evaluation of the patient’s progress and any changes in their condition, the Assessment section must be filled out. This section should be based on the subjective and objective information documented in the previous sections and should include a diagnosis or clinical impression.
Plan Section
Lastly, the Plan section must specify the physical therapist’s treatment plan for the patient. Based on the assessment and specific goals for the patient’s rehabilitation, any interventions or exercises to be implemented must also be discussed. As needed, it must also include any instructions or recommendations for the patient to follow outside of their appointments.
How to Write One
To guide you, heed the following tips for writing effective physical therapy SOAP notes:
Avoid being too vague on the terms you use in describing the patient’s condition or progress.
Use measurable data and observations to support your assessment and treatment plan, and avoid making assumptions or drawing conclusions based solely on subjective information.
Document all relevant information and observations, even if they may seem insignificant at the time. This can help inform your assessment and treatment plan and provide a comprehensive record of the patient’s progress.
Physical Therapy SOAP Note Example
Here’s an example of a physical therapy SOAP note and how it looks like in a sample report when used as a template in SafetyCulture (formerly iAuditor):
Subjective
Trevor Louis Brown is a 45-year-old male who reports low back pain for the past 6 months. Pain is located in the lower back, with a dull ache quality, and moderate intensity. Pain is exacerbated with prolonged sitting and standing, and relieved with rest. No associated signs or symptoms.
Objective
Height: 72 inches
Weight: 200 lbs
BMI: 27.1
Temperature: 98.6°F
Blood Pressure: 126/80 mmHg
General Appearance: Alert and oriented, no signs of distress.
Laboratory Results:
Complete Blood Count (CBC):
Hemoglobin: 14 g/dL (normal range: 13.5-17.5 g/dL)
White Blood Cells (WBC): 7.5 x 10^3/µL (normal range: 4.5-11.0 x 10^3/µL)
Platelets: 200 x 10^3/µL (normal range: 150-400 x 10^3/µL)
Blood Chemistry:
Glucose: 95 mg/dL (normal range: 70-100 mg/dL)
Blood Urea Nitrogen (BUN): 12 mg/dL (normal range: 8-21 mg/dL)
Creatinine: 0.8 mg/dL (normal range: 0.6-1.2 mg/dL)
Sodium: 140 mmol/L (normal range: 135-145 mmol/L)
Potassium: 4.0 mmol/L (normal range: 3.5-5.0 mmol/L)
Assessment
The patient is diagnosed with low back pain, likely due to prolonged standing and heavy lifting at work. The patient has moderate pain intensity with associated activity limitations.
Plan
The patient will undergo a course of physical therapy including stretching and strengthening exercises to improve lumbar flexibility and stability. Modalities such as heat and electrical stimulation may also be used.
Also, the patient will be educated on proper body mechanics to reduce strain on the lower back during work activities. He’ll be advised to avoid activities that aggravate the pain and to continue taking ibuprofen as needed for pain management. The patient will follow up with the therapist in 2 weeks for re-evaluation.
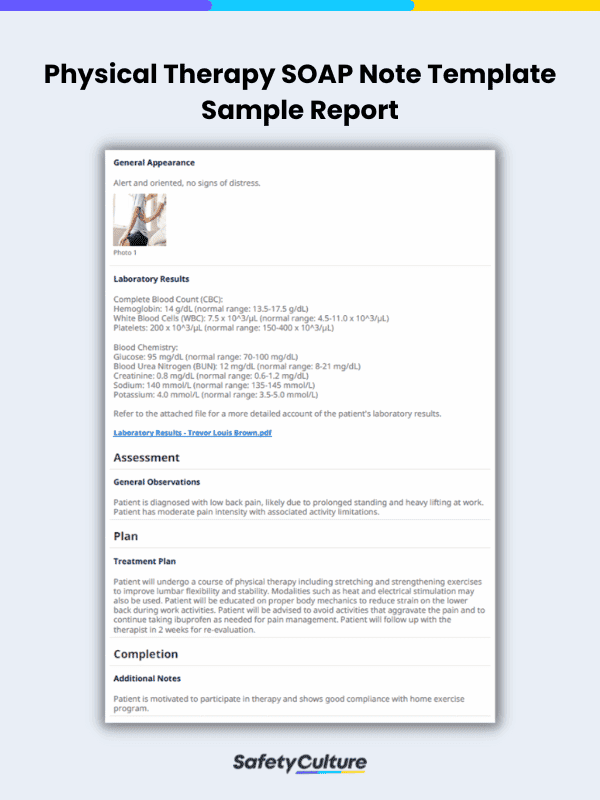
Sample Physical Therapy SOAP Note PDF Report | SafetyCulture
Still looking for a checklist?
Search, filter, and customize 60,000+ templates across industries and use cases.