What is a SOAP Note?
A Subjective, Objective, Assessment, Plan (SOAP) note is a documentation method used by medical practitioners—such as doctors, nurses, pharmacists, and other healthcare practitioners—to assess a patient’s condition. SOAP notes are designed to improve the quality and continuity of patient care by enhancing communication between practitioners and assisting with recall of specific details.
SOAP Note Example – How to Write & What Format
Writing in a SOAP note format allows healthcare practitioners from various fields (e.g., occupational therapy) to conduct clear and concise documentation of patient information. This method of documentation helps the involved practitioner get a better overview and understanding of the patient’s concerns and needs.
Below are SOAP note examples and walkthroughs of how you can effectively write a SOAP note following the SOAP note format depending on your needs:
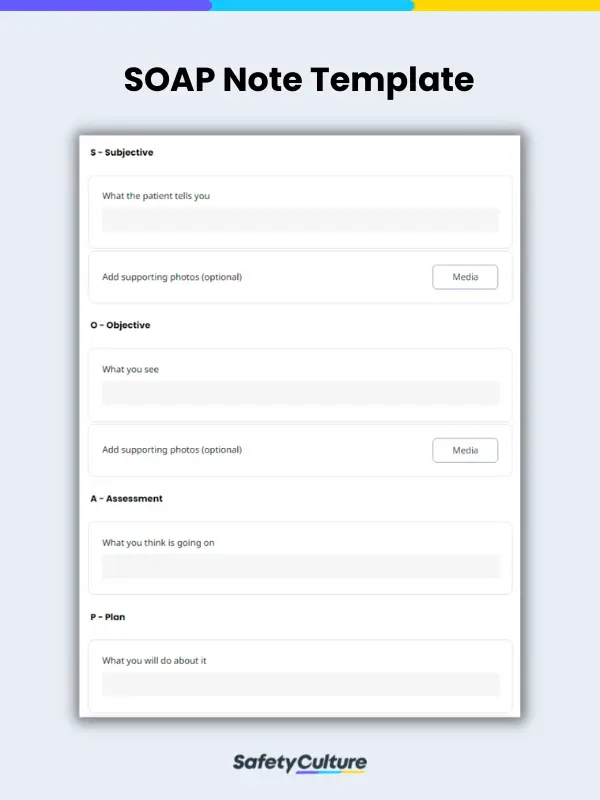
Subjective
What the Patient Tells you
This section refers to information verbally expressed by the patient. Take note of the patient ’s complete statement and enclose it in quotes. Recording patient history such as medical history, surgical history, and social history should also be indicated as it can be helpful in determining or narrowing down the possible causes.
| SOAP Note Example:
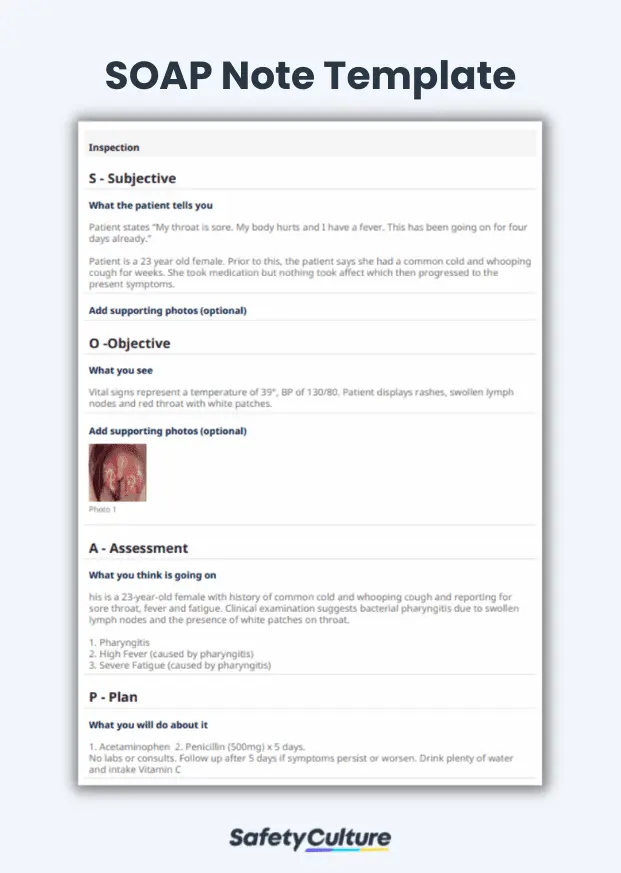
Subjective: Patient states: “My throat is sore. My body hurts and I have a fever. This has been going on for 4 days already.” Patient is a 23-year-old female. Prior to this, patient says she had a common cold and whooping cough then progressed to the current symptoms. |
Objective
What You See
This section consists of observations made by the clinician. Do a physical observation of the patient’s general appearance and also take account of the vital signs (i.e temperature, blood pressure etc). If special tests were conducted, the results should be indicated in this section. Using the previous example, we can write the objective like this:
| SOAP Note Example:
Objective: Vital signs represent a temperature of 39°, BP of 130/80. Patient displays rashes, swollen lymph nodes and red throat with white patches. |
Assessment
What You Think is Going on
This section tells the diagnosis or what condition the patient has. The assessment is based on the findings indicated in the subjective and objective section. This section can also include diagnostic tests ordered (i.e x-rays, blood work) and referral to other specialists. Using the same example, the assessment would look like this:
| SOAP Note Example:
Assessment: This is a 23-year-old female with a history of common cold and whooping cough and reporting for a sore throat, fever, and fatigue. Clinical examination suggests bacterial pharyngitis due to swollen lymph nodes and the presence of white patches on the throat.
|
Plan
What You Will Do About It
This section addresses the patient’s problem identified in the assessment section. Elaborate on the treatment plan by indicating medication, therapies, and surgeries needed. This section can also include patient education such as lifestyle changes (i.e food restrictions, no extreme sports etc). Additional tests and follow up consultations can also be indicated. With the same example, the plan section can be written like this:
| SOAP Note Example:
Plan:
|
FAQs About SOAP Notes
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan which are the four parts of a SOAP note. All four parts are designed to help improve evaluations and standardize documentation:
- Subjective – What the patient tells you
- Objective – What you see
- Assessment – What you think is going on
- Plan – What you will do about it
Yes, It is still widely being used in modern clinical practice. Whether in paper or digital format, a soap note is one of the tools used by healthcare institutions for documenting and communicating patient information.
SOAP note helps in providing succinct yet thorough and relevant medical information about the patient. Other benefits include:
- It makes tracking of the patient’s progress easier
- Keeps patient’s medical data organized
- Enhances care coordination between healthcare professionals
SOAP notes are often written following the order or format of Subjective, Objective, Assessment, and Plan. There are instances, however, where rearranging them is necessary and more beneficial depending on the information that is most relevant to the situation. An example would be to follow the APSO format which allows healthcare professionals to prioritize their assessment and plan, emphasizing the diagnosis, treatment, and management decisions.
SOAP notes include data such as the client’s medical history, chief complaint, or what the patient tells you (Subjective); laboratory results, physical examination, and other measurable data, or what you actually see (Objective); clinical assessment, diagnosis, or what you think is going on (Assessment); and the proposed plan or treatment for the patient, or what you plan to do about it (Plan).