What is a Mental Health SOAP Note Template?
A mental health Subjective, Objective, Assessment, and Plan (SOAP) note template is a document used by those in healthcare, counseling, and mental health support to document a patient’s mental health status and the care provided during each session. With a SOAP note template specifically for mental health care, you can help better understand your patient’s issues, needs, and how to best help them.
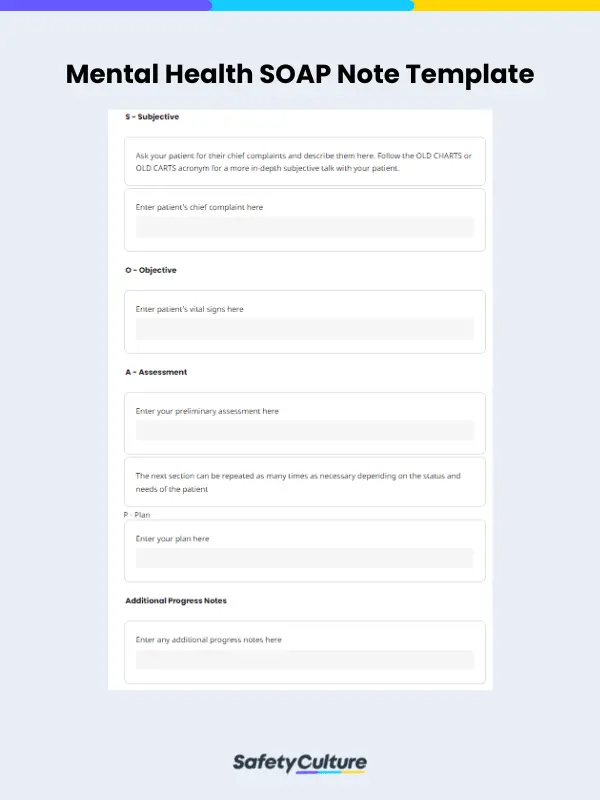
What to Include in a Mental Health SOAP Note Template and How to Use One
A mental health SOAP note template has one section each for the elements of SOAP. In some cases, in addition to these four sections, a well-designed template may include a fifth section for Progress notes. Each section provides a unique perspective on the patient’s mental health status and helps the healthcare provider to track changes over time.
The main purpose of each section serves a specific role in documenting a patient’s mental health status and the care provided during each session.
Subjective
The Subjective section will be for the patient’s chief complaint (CC). Here, you will input the information that the patient provides about their mental health status, such as symptoms, feelings, and concerns. This allows you to understand the patient’s perspective and provides valuable information for assessing the patient’s mental health status.
When filling up the subjective portion and talking to your patient, use the OLD CHARTS or OLD CARTS acronym as a basis to get a full view of their medical and counseling history and complaints. OLD CHARTS or OLD CARTS stands for:
- Onset: When did the CC or symptoms first start? When did each symptom first start?
- Location: Where is the CC felt, or where on the body does it manifest?
- Duration: How long has the patient been dealing with their CC?
- Character: How does the patient describe their CC?
- Alleviating or Aggravating Factors: What behaviors, acts, and environmental factors increase or decrease the patient’s CC or symptoms? What actions or interactions reduce or increase the severity of the patient’s symptoms?
- Radiation: Is the patient’s CC only felt in one or a few parts of the body?
- Temporal Pattern: Does the patient’s CC only hurt or appear during certain times of the day or after certain activities?
- Severity: On a scale of 1 to 10, how would the patient rate the pain and impact their CC has on their life?
Objective
This section is for inputting factual information about the patient’s mental health status, such as their vital signs, physical exam findings, and your observations of their behavior. With this section, you can see all the objective views of the patient’s mental health status, which helps the healthcare provider identify any physical or behavioral changes that may require further evaluation.
If possible, also ask your patient for their past mental health records and their previous doctors’ or counselors’ reports. While these documents may no longer be valid, having them can give you a more holistic view of your patient’s objective history.
Assessment
The Assessment section will be your space to input your professional assessment of your patient’s mental health status based on the information gathered in the previous sections. This section will help you create a diagnosis, identify other potential risks and concerns, and develop the right treatment plan for your patient.
Plan
The Plan section includes your plan for addressing and treating your patient’s mental health condition. This section contains plans for medications, therapy, or referrals to other healthcare professionals who may better help your patient. The Plan section aims to provide a clear and organized plan for the patient’s treatment to help you track their progress and make adjustments as needed.
Depending on the situation, if your patient is experiencing multiple conditions as a result of different complaints, your notes should include separate plans for each one. After each new visit, these plans should be revisited and adjusted.
In some cases, an additional Progress Notes section may be added to your Plan section. This section will include updates on the patient’s progress over time, such as any changes in symptoms, treatments, or other relevant information.
Benefits
Using a SOAP note template in addressing mental health issues has several benefits. Most importantly, it can save time and improve efficiency by providing a standardized format for note-taking. This can help healthcare professionals quickly and easily document important patient information without the need for extensive note-taking, as well as ensure that all necessary components of the note are included.
Additionally, using a SOAP note template can improve communication among healthcare professionals by providing a consistent format for sharing information. This can improve collaboration and ensure that all members of the healthcare team are on the same page regarding the patient’s care.
With a mental health SOAP note template in a digital form, your benefits will also increase. By using a digital solution, you can also:
- Access your mental health SOAP notes anytime and anywhere
- Ensure your documents are protected from tears and storage problems by storing them in the cloud instead
- Coordinate with your organization and other professionals you work with in-app regarding possible issues with your patient and care plans
- Streamline your workflow processes and your patient’s recovery by digitizing all your processes
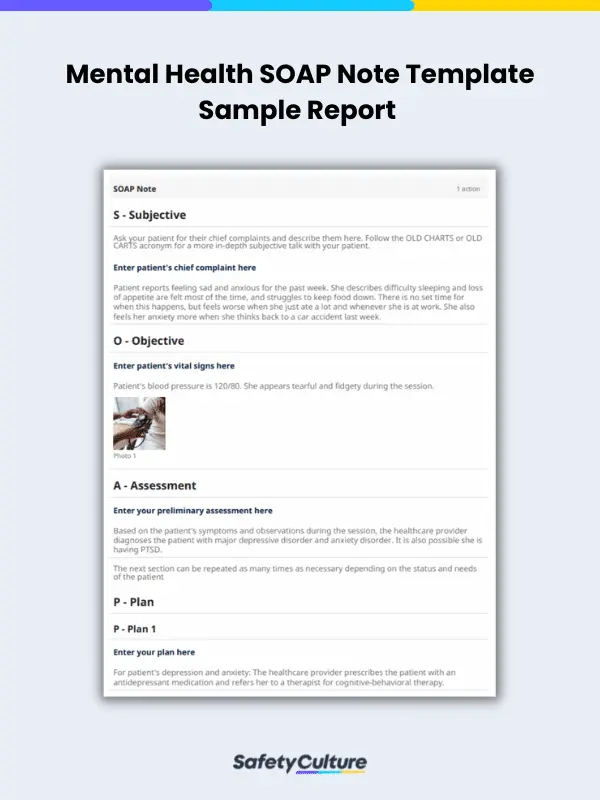
Example Report
Here is a sample report of a mental health SOAP note template filled out for your reference:
FAQs about Mental Health SOAP Note Templates
Yes, social workers can use mental health SOAP note templates in their daily work. However, not all social workers may be equipped to use them or be well-versed in mental health topics, so they should be educated first on them.
Using a SOAP note is not the only way to conduct and provide mental health counseling, but it is one of the best ways to do so. This is because a SOAP note, particularly a mental health SOAP note template, is one of the most versatile and easy-to-use tools available for collecting and collating information.
Behavior, Intervention, Response, Plan (BIRP) notes and SOAP notes are both tools meant to help mental health professionals streamline their note-taking processes. Their main difference is that a BRIP note focuses on describing a counseling session’s theme, while SOAP notes aim to be more objective and are more focused on future treatment plans.