What are Pediatric SOAP Notes?
Pediatric SOAP notes are structured formats used by healthcare professionals to document a child’s medical information in a concise and organized manner. SOAP stands for Subjective, Objective, Assessment, and Plan, and each component serves a specific purpose. Pediatric SOAP notes provide a standardized method of documenting patient information, allowing for accurate communication between healthcare professionals and reducing the risk of errors.
Why Use One
Pediatric SOAP notes help ensure the continuity of care given to pediatric patients through the following ways:
1. Standardization of Documentation
Using a pediatric SOAP note template standardizes the documentation process for all healthcare providers. It ensures that everyone documents patient information consistently, making it easier to read and understand the notes. This also ensures that all necessary details are included, which can be crucial in an emergency situation.
2. Improved Communication Among Healthcare Providers
When healthcare providers use the same format for documentation, it makes it easier to communicate with one another. A pediatric SOAP note template provides a structured format that makes it easy to understand what is happening with the patient, the course of treatment, and the expected outcome.
3. Improved Quality of Care
It can also help enhance the quality of treatment and care provided to pediatric patients. A structured format ensures that all accurate data is captured, and healthcare providers can use them to make informed decisions and plan effective interventions.
What to Include in a Pediatric SOAP Note
As healthcare professionals, creating accurate and comprehensive medical records is an essential part of providing quality care to patients. To help ensure this, the following sections must be well-written in a pediatric SOAP note:
Subjective Section
The Subjective section is where you document the patient’s chief complaint and any relevant information that the patient or their caregiver provides. This section provides insight into the patient’s symptoms, concerns, and overall health status. It’s also an opportunity to build rapport with the patient and establish trust, which is especially important when working with pediatric patients.
When writing the Subjective section, use clear and concise language and document the information in a logical and organized manner. With that, here are some tips you can follow:
- Begin by stating the patient’s chief complaints in their own words. This helps to ensure that you are addressing the patient’s primary concern and can guide the rest of the note.
- Ask open-ended questions to gather additional details about the patient’s symptoms and concerns. This way, you can uncover any underlying issues that may be contributing to the patient’s condition.
- Document any relevant medical history, including past illnesses, surgeries, and medications to provide important context for the patient’s current condition.
- Use the appropriate medical terminology, but avoid using jargon that the patient or caregiver may not understand.
- Be empathetic and listen carefully to the patient’s concerns. This can help to build trust and establish a positive relationship with the patient.
Objective Section
This section is used to document the objective findings from the physical examination and any diagnostic tests or imaging studies. The healthcare provider should document vital signs, including the patient’s temperature, heart rate, respiratory rate, blood pressure, and oxygen saturation.
This section should be written in objective language, using precise medical terminology and standard abbreviations and ensuring it’s concise and accurate.
Assessment Section
After collecting the subjective and objective data, the Assessment section is where the healthcare provider documents their assessment and diagnosis of the patient’s condition. This information will then be used when creating the plan of care.
Plan Section
Lastly, the plan should be tailored to the patient’s specific needs, taking into account their medical history, physical examination findings, and assessment. The plan should also be evidence-based, supported by relevant data and information, and includes any referrals the healthcare provider made.
Additionally, the healthcare provider should document any patient education that they provided to the patient or their caregivers. Patient education is a critical component of the plan of care since the patient and their caregivers must understand their condition, treatment options, and any potential side effects or complications.
How to Write One: General Tips
To ensure a well-written pediatric SOAP note, here are some general tips to follow:
- Use clear, concise language and avoid unnecessary details.
- Ensure that all relevant information is included in the note, including the patient’s medical history, physical examination findings, assessment, and plan of care.
- Use objective language when documenting the physical examination findings and assessment. Avoid subjective terms and opinions.
- Tailor the care plan to the patient’s specific needs and take into account any comorbidities, contraindications, or patient preferences.
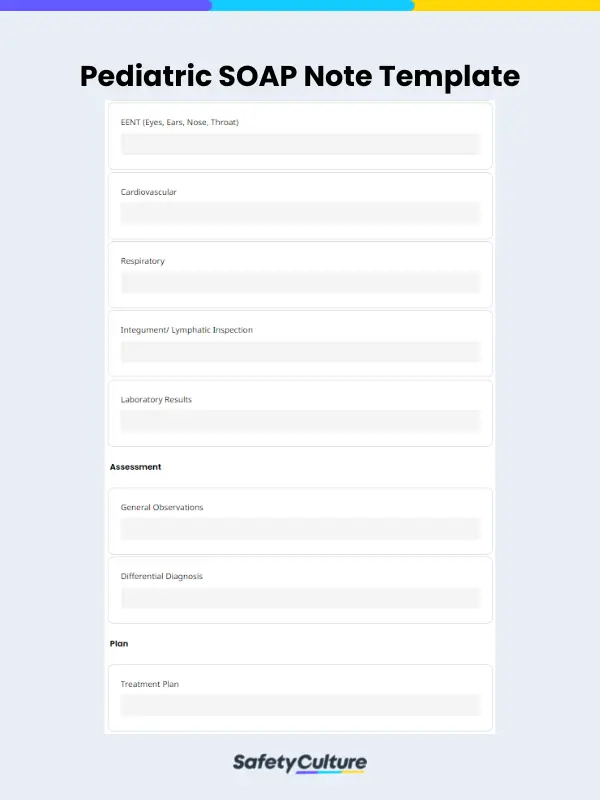
Pediatric SOAP Note Example
Here’s an example of a pediatric SOAP note and how it looks like in a report generated using a template in SafetyCulture (formerly iAuditor):
Subjective
Sarah Smith is an 8-year-old female who presents with a severe headache and nausea. The patient rates the headache as an 8 out of 10 in severity and notes that it started suddenly one day ago. The headache is located in the frontal area and is accompanied by nausea and vomiting. There are no known factors that alleviate or aggravate the headache, and there are no associated signs or symptoms.
Objective
Physical Examination – Vital Signs:
- Height: 50 inches
- Weight: 65 pounds
- BMI: 22.2
- Temperature: 99.1°F
- Blood Pressure: 110/70 mmHg
General: Sarah appears uncomfortable due to her headache, but her general appearance is otherwise normal.
EENT:
- Eyes: PERRLA, visual fields intact, no conjunctival injection
- Ears: Normal external canals, tympanic membranes clear
- Nose: Normal nares, turbinates, and septum
- Throat: Normal oral mucosa and posterior pharynx
Cardiovascular: Heart sounds are normal, with no murmurs or gallops.
Respiratory: The lung sounds are clear.
Integument/Lymphatic: The skin is intact with no lesions or rashes.
Assessment
Based on Sarah’s symptoms and physical examination, the likely differential diagnosis includes migraines, tension headaches, and viral infections.
Plan
Sarah will be treated with ibuprofen for her headache, and her symptoms will be monitored closely. If her symptoms persist or worsen, further diagnostic tests may be necessary. In the meantime, Sarah is advised to rest and avoid strenuous activity.
Follow-up: The patient will follow up in 2 days to evaluate the effectiveness of the treatment plan and any changes to her symptoms.
Education: The patient and family will be educated about the possible causes of headaches in children, including stress, lack of sleep, and dehydration. They will also be advised on the importance of rest and hydration to prevent future headaches.
FAQs About Pediatric SOAP Notes
Pediatric SOAP notes are typically written by healthcare providers who work with pediatric patients, such as pediatricians, pediatric nurse practitioners, or pediatric physician assistants. They’re also in charge of ensuring that only legitimate and accurate information is stated therein.
In most cases, parents or caregivers can request access to their child’s pediatric SOAP notes. However, healthcare providers may have specific policies or procedures in place for how to request and access medical records to uphold privacy security and confidentiality as needed.
The length of time that pediatric SOAP notes are kept on file may vary depending on the healthcare provider or organization. In general, medical records must be retained for a certain period of time like 10 years, or as required by law or regulation.
Yes, pediatric SOAP notes are considered confidential medical records and are protected under federal and state privacy laws, such as the Health Insurance Portability & Accountability Act (HIPAA). Only authorized individuals, such as the patient or their legal guardian, have access to the medical record.