What are BIRP Notes?
A BIRP note is a documentation format that covers 4 areas: Behavior, Intervention, Response, and Plan. It gives a framework for recording observations, actions, responses, future sessions, and other essential information during client interactions. This note-taking structure is used in psychiatry, psychology, counseling, and similar fields to ensure comprehensive recordkeeping and streamline information-sharing among health providers.
Benefits of Using Them
Structured note-taking is crucial for maintaining accurate and consistent records of therapy sessions. Following a standardized framework like BIRP notes allow therapists, counselors, and mental health professionals to gather essential information, progress, and changes observed during each session. This way, they can devise strategies that work for their patient’s needs and conditions.
Aside from this, using BIRP notes and similar medical documentation formats offer the following benefits:
- Clear communication – These notes give a clear and concise overview of the patient’s progress, making it easier to share vital information with other healthcare professionals involved in the patient’s care.
- Efficient treatment planning – Mental health professionals can analyze their findings on the BIRP notes to identify behavioral patterns and areas that require attention. Using this information, they can devise treatment plans tailored to the specific needs and goals of the client.
- Evaluation of interventions – BIRP notes also allow therapists, counselors, and similar professionals to assess the effectiveness of the interventions employed during sessions. They can review the recorded responses to make informed decisions about adjusting, continuing, or halting treatment approaches according to what works best for the client.
- Measurement of progress – Lastly, BIRP notes are useful for tracking the progress of the client over time and finding potential blockers and areas for improvement. This process ensures that treatment plans are modified to meet the intended goals.
How to Write BIRP Notes
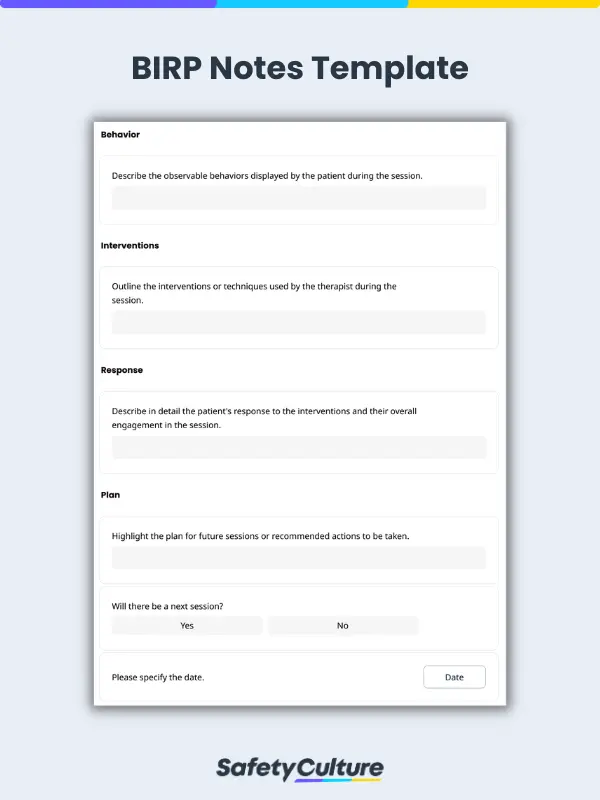
Just as the name suggests, BIRP notes follow a specific format with 4 components: Behavior, Intervention, Response, and Plan. Here are the steps on how to write each of these sections:
Behavior
Begin the BIRP note with a description of the specific behaviors displayed by the client during the session. This section helps identify the problem to be addressed during the session, better understand the client’s current state, and determine behavioral patterns and changes over time.
When writing this section, here are a few things to consider:
- Take note of observable actions, emotions, statements, and nonverbal cues.
- Provide context for the behavior, such as the client’s mood, environment, or triggers.
- Include the client’s account of how they’re feeling outside of the session.
Interventions
After noting the client’s behavior during and outside the session, the next step is to outline the actions, strategies, or techniques employed to address the identified behavior. When writing this section, it’s best to:
- Specify the therapeutic techniques used (e.g., cognitive-behavioral therapy, mindfulness exercises, motivational interviewing).
- Describe how the method of intervention was implemented and why it was selected.
- Explain how the chosen approach connects with the overall treatment plan for the client.
Response
This section details how the patient has reacted or responded to the interventions used during the session. Essentially, it answers the question, “Did the approach address the problem being targeted?”
Consider the following points when recording their response:
- Evaluate the effectiveness and impact of the intervention on the patient’s emotions and behavior.
- Gauge the response using measurable benchmarks, such as improved coping skills, reduced anxiety levels, or increased self-awareness.
- Document any feedback that the patient has given regarding the intervention and its perceived effectiveness.
Plan
Once you’ve collected all vital information from the previous sections, the final step is to map out the next steps and future course of action. Be sure to include the following items in this section:
- Date and time of the succeeding scheduled sessions
- Timeline for reviewing the plan’s effectiveness
- Referrals or appointments to other physicians or specialists
- Home assignments to the patient (if any)
- Other follow-up actions related to the patient’s treatment plan
BIRP Notes Example
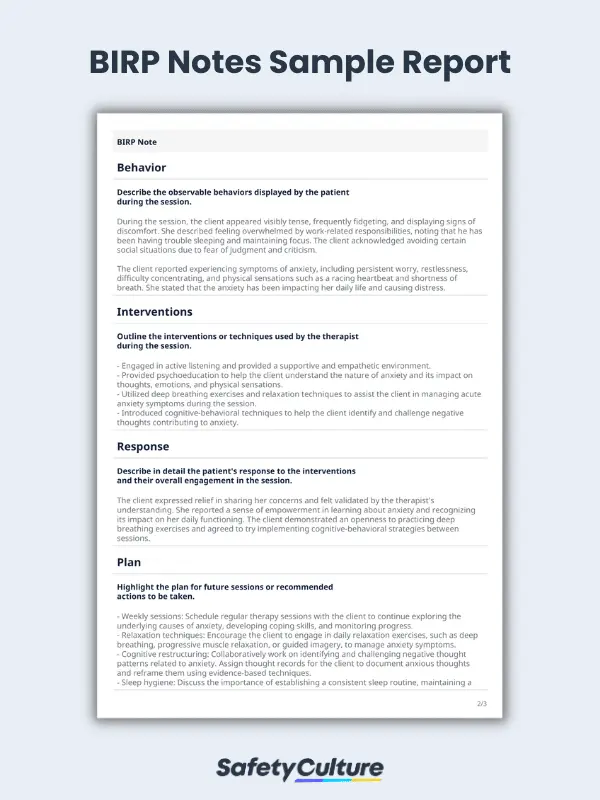
To illustrate how things work, here’s a sample BIRP note used in mental health settings:
Behavior:
During the session, the client appeared visibly tense, frequently fidgeting, and displaying signs of discomfort. She described feeling overwhelmed by work-related responsibilities, noting that he has been having trouble sleeping and maintaining focus. The client acknowledged avoiding certain social situations due to fear of judgment and criticism.
The client reported experiencing symptoms of anxiety, including persistent worry, restlessness, difficulty concentrating, and physical sensations such as a racing heartbeat and shortness of breath. She stated that the anxiety has been impacting her daily life and causing distress.
Interventions:
- Engaged in active listening and provided a supportive and empathetic environment.
- Provided psychoeducation to help the client understand the nature of anxiety and its impact on thoughts, emotions, and physical sensations.
- Utilized deep breathing exercises and relaxation techniques to assist the client in managing acute anxiety symptoms during the session.
- Introduced cognitive-behavioral techniques to help the client identify and challenge negative thoughts contributing to anxiety.
Response:
The client expressed relief in sharing her concerns and felt validated by the therapist’s understanding. She reported a sense of empowerment in learning about anxiety and recognizing its impact on her daily functioning. The client demonstrated an openness to practicing deep breathing exercises and agreed to try implementing cognitive-behavioral strategies between sessions.
Plan:
- Weekly sessions: Schedule regular therapy sessions with the client to continue exploring the underlying causes of anxiety, developing coping skills, and monitoring progress.
- Relaxation techniques: Encourage the client to engage in daily relaxation exercises, such as deep breathing, progressive muscle relaxation, or guided imagery, to manage anxiety symptoms.
- Cognitive restructuring: Collaboratively work on identifying and challenging negative thought patterns related to anxiety. Assign thought records for the client to document anxious thoughts and reframe them using evidence-based techniques.
- Sleep hygiene: Discuss the importance of establishing a consistent sleep routine, maintaining a relaxing sleep environment, and implementing relaxation techniques before bedtime.
- Referral: Explore the possibility of referring the client to a psychiatrist for a comprehensive evaluation of her symptoms and potential consideration of medication, if deemed necessary.
Best Practices for Creating These Notes
When writing BIRP notes, it’s a must to pay attention to details, adhere to ethical guidelines, and ensure accuracy in your notes. Here are some best practices that you can follow to improve the quality and effectiveness of your notes:
- Use clear, concise, and objective language when writing your notes.
- Instead of using jargon and ambiguous terms, focus on the specific details and precise descriptions of behaviors, interventions, responses, and plans.
- Highlight the most significant behavioral observations, notable interventions, noteworthy responses, and essential components of the treatment plan.
- Promptly complete these notes after each session to ensure timeliness and accuracy of information.
- Establish appropriate security measures to protect the client’s confidentiality.
- Only share information with authorized professionals involved in the client’s care.
FAQs about BIRP Notes
Both SOAP and BIRP notes offer a standardized way of documenting patient visits but differ in terms of structure and approach. BIRP notes highlight behaviors and responses, making them ideal for mental health assessments. On the other hand, SOAP notes capture both objective and subjective information, making them suitable for comprehensive medical notes.
Generally, BIRP notes are meant to be concise yet comprehensive enough to record essential behavioral observations, interventions, responses, and plans. However, some cases may call for long BIRP notes, such as modifications in the treatment plan and assessments of multiple risk factors.
In most cases, it’s recommended to update BIRP notes at least once per session to ensure accurate and up-to-date information. However, this frequency can change depending on the specific needs and requirements of the individual and mental health setting.
Using BIRP notes comes with its own set of challenges, including the following:
- Keeping consistent and standardized documentation across different practitioners
- Recording behaviors and responses accurately and objectively
- Managing the time required to write detailed notes
- Ensuring privacy and confidentiality when documenting sensitive information