What is a COVID Risk Assessment Tool?
A COVID risk assessment tool is used to measure the likelihood of a person or a group of people (as in a business or any other institution) of contracting COVID-19. Unlike a COVID test, which is an instrument or procedure used to identify the presence of the virus at the time of the test, a COVID risk assessment tool determines vulnerability and is designed to help identify persons who are at risk of acquiring COVID-19. By identifying those most at risk, a COVID risk assessment tool allows them and the people around them to take the necessary steps to protect themselves and curb the spread of the coronavirus.
What are the COVID-19 Risk Factors?
While the risk factor with the most impact overall (in terms of COVID-19 infection, hospitalization, and death) is age, there are a number of other known risk factors such as race/ethnicity and certain medical conditions. According to the CDC (Centers for Disease Control and Prevention), specific ethnicities have a higher risk of COVID-19 infection compared to others. Data has also shown that adults who are pregnant, smoking, obese, severely obese or with Type 2 diabetes, heart conditions, immunocompromised state from solid organ transplant, chronic kidney disease, chronic obstructive pulmonary disease, sickle cell disease, down syndrome, and cancer are at an increased risk of severe illness from coronavirus, regardless of age.
The CDC also notes that individuals with any underlying medical condition (even those not stated above) should consult with their doctors regarding their personal risk factors including age, race/ethnicity, gender, and use of certain medications. Non-personal risk factors, such as certain occupations, poverty, and overcrowding, have been identified by the CDC, but the exact nature of these risks is much more difficult to specify due to the wide variety of jobs, workplaces, and living situations. Despite these challenges, non-personal risk factors should also be considered because limiting the scope to personal risk factors doesn’t provide the bigger picture and may lead to missed opportunities to discover more about the virus and how it spreads.
Important non-personal risk factors that COVID risk assessment tools should incorporate are the following:
- High-risk setting (during a pandemic surge) and low-risk setting (in between surges)
- Local viral transmission rates (including variation in community prevalence)
- How the individual commutes
- Workplace factors (disease prevalence within facilities or workplace behaviors)
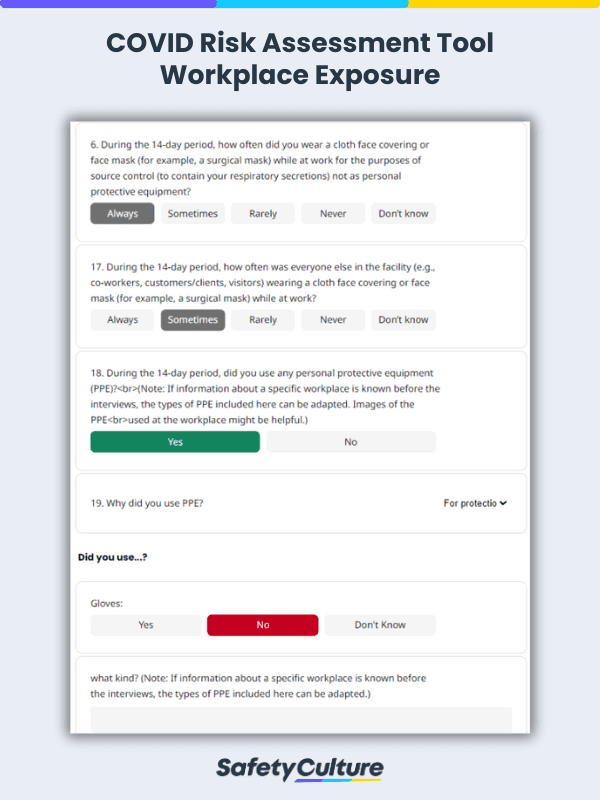
- Strength of mitigation measures (inability to isolate infected workers or lack of PPE)
COVID-19 (Coronavirus) Vaccines
At the time of writing, there are only three COVID-19 vaccines authorized and recommended for use in the United States. These are the Pfizer-BioNTech COVID-19 vaccine, the Moderna COVID-19 vaccine, and Johnson & Johnson’s Janssen COVID-19 vaccine.
Since the Pfizer-BioNTech COVID-19 vaccine and the Moderna COVID-19 vaccine are of the same vaccine type (mRNA), they share many similarities, including side effects and recommendations on who should not receive the vaccines. Those who have had a severe allergic reaction or an immediate allergic reaction to any ingredient in an mRNA COVID-19 vaccine or are allergic to PEG or polysorbate should not receive an mRNA COVID-19 vaccine.
The most common side effects of these two vaccines are pain, swelling, and redness in the arm where the vaccine was injected, headache, chills, and tiredness throughout the rest of the body. According to the CDC, these side effects start within a day or two of getting the vaccine, but should subside in a few days.
Unlike the Pfizer-BioNTech COVID-19 vaccine and the Moderna COVID-19 vaccine, Johnson & Johnson’s Janssen COVID-19 vaccine is of a different vaccine type known as a viral vector. However, similar to the previous two vaccines, those who have had a severe allergic reaction to any ingredient of the Janssen vaccine should not receive it.
The Janssen vaccine also has more or less the same side effects as the Pfizer-BioNTech COVID-19 vaccine and the Moderna COVID-19 vaccine. According to the FDA Fact Sheet for Recipients and Caregivers, side effects of the Janssen COVID-19 vaccine include:
- Injection site reactions: pain, redness of the skin, and swelling.
- General side effects: headache, feeling very tired, muscle aches, nausea, and fever.
Taking all of these things into consideration, the benefits of receiving COVID-19 vaccination far outweigh the risks, unless one has had an allergic reaction to any of the vaccine ingredients or is confirmed to be allergic to PEG or polysorbate.
Assessing Asymptomatic Close Contacts
If any employee is suspected or confirmed to have COVID-19, evaluate first which employees have had possible close contact (within 6 feet for a cumulative total of 15 minutes or more over a 24-hour period) with said person and inform them immediately while maintaining confidentiality as required by the Americans with Disabilities Act or any other applicable law.
CDC recommends instructing potentially exposed employees to stay home for 14 days and self-monitor for symptoms, even if both the employee suspected or confirmed to have COVID-19 and their close contacts were wearing masks and were not experiencing any symptoms at the time of exposure. This recommendation is based on growing evidence of transmission risk from infected people without symptoms (asymptomatic) or before the onset of recognized symptoms (presymptomatic).
Logistics Challenges of Infection Control
If it has been less than 7 days since an employee suspected or confirmed to have COVID-19 has been in the workplace, close off any areas used for prolonged periods of time by said person, open outside doors and windows to increase air circulation in these areas, and wait 24 hours before cleaning and disinfecting.
Here are a few additional steps to take to reduce or stop the spread of coronavirus in the workplace:
- Increase physical space between employees through the placement of partitions.
- Assign someone to clean and disinfect surfaces.
- Schedule handwashing breaks.
- Provide flexible sick leave policies.
Implementing such infection control procedures can be tedious and overwhelming, especially for employers in industries where telework or working remotely is not possible. In the end, similar to receiving COVID-19 vaccination, the benefits of these safety measures far outweigh the risks. Aside from the personal effects of a COVID-19 outbreak on the lives of employees, its impact on overall business operations should not go unnoticed, nor should it be underestimated.