- Home
- Checklist PDF
SOAP Note Template PDF
6 Free SOAP Note PDF Form & Templates
Downloadable SOAP note templates designed to help healthcare professionals document and evaluate a patient’s condition
Here’s a collection of SOAP Note templates that are used in various areas of the healthcare industry:
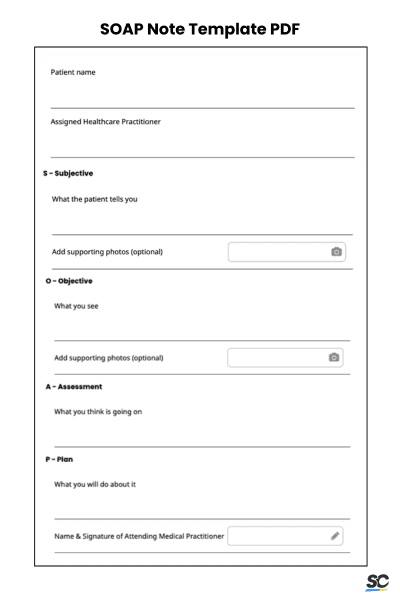
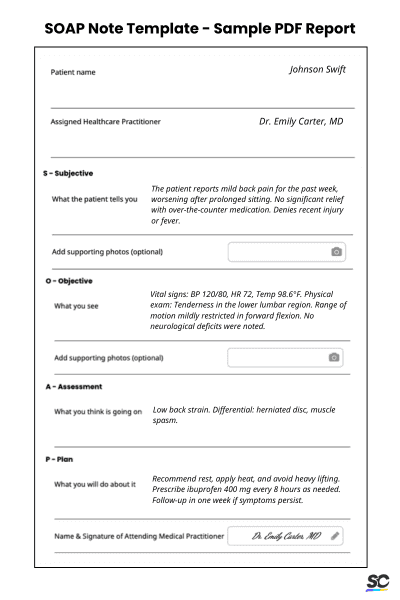
1. SOAP Note Template PDF
This generic clinical SOAP note template can be used across all areas encompassing healthcare. With this template, you’ll be able to
Fill out essential information such as the patient name, assigned medical practitioner, and date of assessment
Fill out subjective assessment based on what the patient says
Fill out the objective section based on what you see during the observation
2. SOAP Note Template Mental Health PDF
As the name suggests, this template is used specifically for mental health assessments. This can also serve as a data collection tool that can help therapists and counselors understand their patients.
Log initial information such as patient name and date of assessment
Write down the chief complaint of the patient—try to be as detailed as possible
Add in any progress notes that are not mentioned in the first part of the document
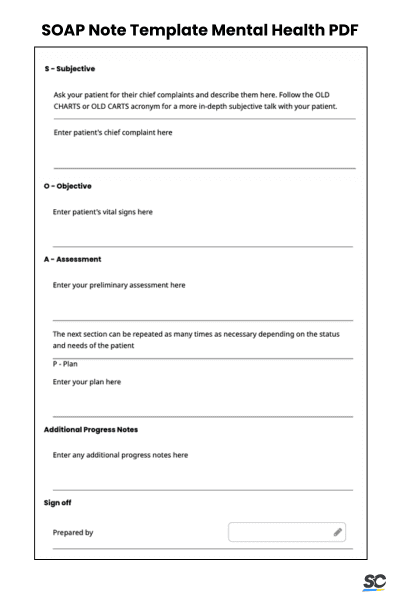
SOAP Note Template Mental Health PDF
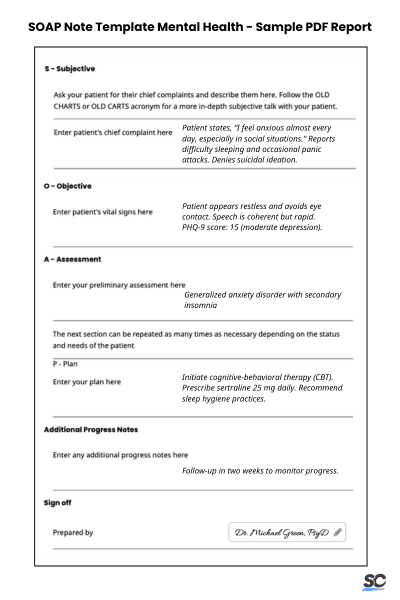
SOAP Note sample PDF report for mental health assessment
3. Nursing SOAP Note Template PDF
Nurses best use this detailed SOAP note as it allows them to collect patient information thoroughly. With this PDF template, nurses can do the following:
Ask about past medical history and the patient’s current illness, as well as family history
Detail important aspects such as blood pressure, general appearance, and laboratory results
Add in general observations and plans
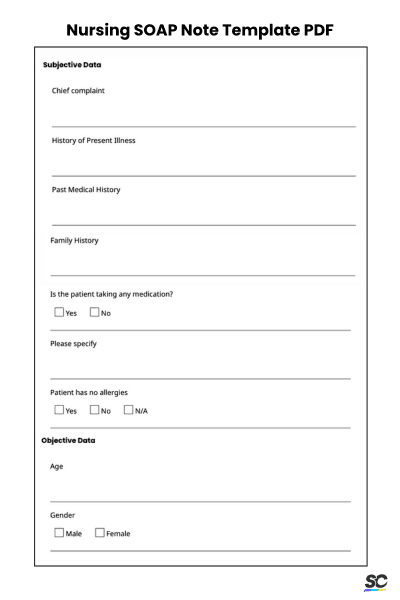
Nursing SOAP Note Template PDF
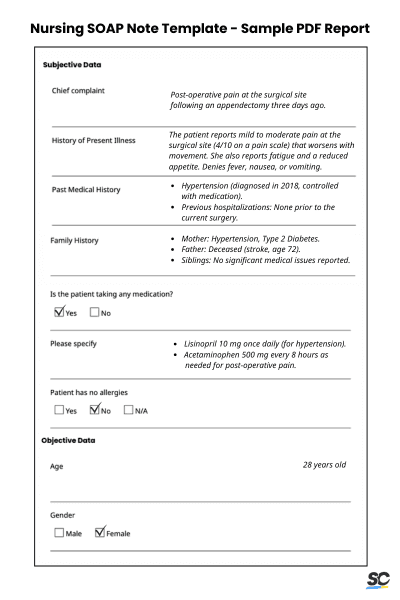
SOAP Note sample PDF report for nurses
4. Pediatric SOAP Note Template PDF
Pediatricians best use this ready-to-use SOAP note PDF template for their child patients. Pedias can use this template to document a patient’s medical data and record current observations they may have. With this template:
List down important information such as age, chief complaint, and past medical history
Get the child’s height, weight, BMI, and laboratory results
Detail the overall assessment and diagnosis
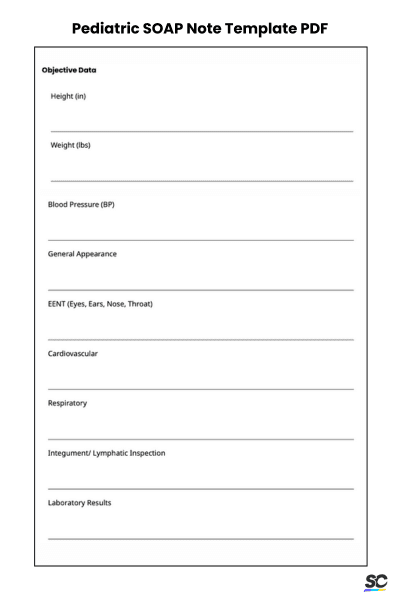
Pediatric SOAP Note Template PDF
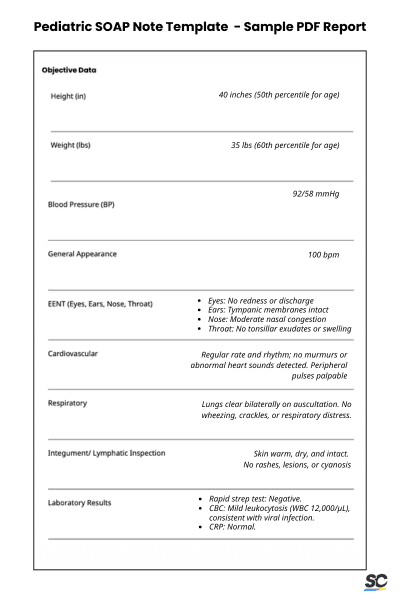
SOAP Note sample PDF report used by pediatricians
5. Physical Therapy SOAP Note Template PDF
This SOAP note PDF template is designed for physical therapists. They can use this checklist to standardize patient documentation by ensuring that assessments are recorded in a structured format. Further, this template enables them to:
Use detailed notes to tailor treatment plans to the patient’s specific needs
Adjust interventions based on observed outcomes
Offer detailed evidence of the care provided to justify insurance claims or billing
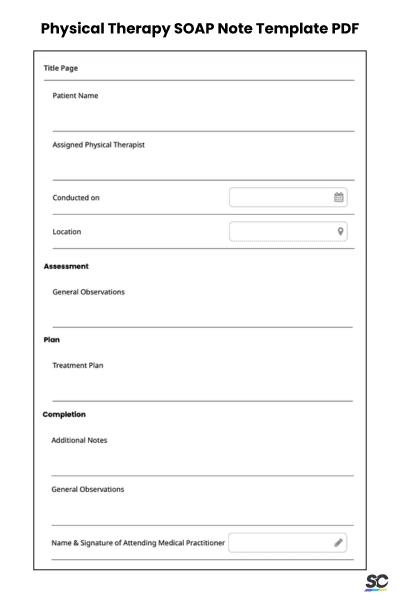
Physical Therapy SOAP Note Template PDF
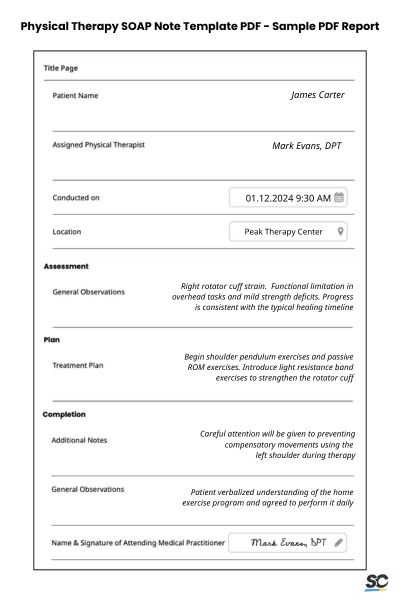
SOAP Note sample PDF report for physical therapy
6. Occupational Therapy SOAP Note Template PDF
This occupational therapy SOAP note template is designed to streamline the documentation of patient care by organizing subjective observations, objective measurements, and diagnostic information. Further, this template helps users to:
Document patients’ primary concerns and assess their physical and functional status
Analyze data to address these concerns
Come up with evidence-based intervention plans tailored to individual needs
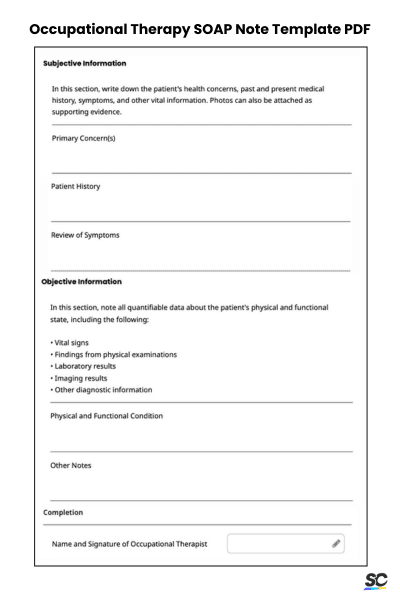
Occupational Therapy SOAP Note Template PDF
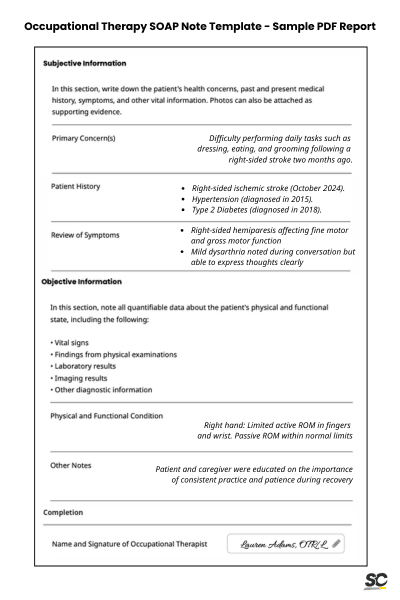
SOAP Note sample PDF report for occupational therapy
Why Use PDF SOAP Note Templates?
Using PDF SOAP note templates ensures consistency and structure in documentation, making them invaluable for professionals who need to record client or patient interactions. The SOAP format—comprising Subjective, Objective, Assessment, and Plan—provides a standardized approach that helps streamline note-taking while ensuring all critical aspects are covered.
PDFs are especially beneficial because unless manually modified, they remain consistent, making them reliable and easy to use. All these advantages ultimately help ensure compliance with standards and requirements.
How to Use SOAP Notes PDF Templates
Here’s a step-by-step instructions on how to use PDF templates for SOAP Notes:
Identify relevant SOAP Note template – Access and download a SOAP note PDF template compatible with your documentation needs.
Fill out subjective and objective sections – Begin by completing the Subjective section with the patient’s reported symptoms, concerns, or medical history. Then, record measurable and observable data in the Objective section, such as vital signs, lab results, or physical exam findings.
Write the assessment – Summarize your interpretation or diagnosis based on the information from the Subjective and Objective sections. Be concise while addressing the key findings.
Detail the plan – Outline the next steps, including treatment recommendations, prescribed medications, follow-up actions, or referrals to other specialists. Ensure the plan is clear and actionable.
Save and store – Once the note is complete, save the file securely on your device or patient management system. If using a printed version, file it in the patient’s physical record for easy retrieval.
Customize Your SOAP Note PDF Template
Aside from using pre-existing SOAP note templates, healthcare professionals can also try to customize their own based on specific needs. This is especially useful if there are specific areas that they want to emphasize. For example, practitioners can add dedicated areas for patient education, medication tracking, follow-up reminders, or risk assessment.
This flexibility ensures that the documentation aligns with the unique requirements of a practice or specialty, enabling a more detailed and comprehensive clinical assessment. Custom templates also encourage consistency in recording data, helping healthcare teams communicate critical information. By adapting SOAP notes to their workflow, professionals can enhance the quality of care and maintain thorough, personalized records.
Explore a Digital Solution for SOAP Note Assessments
Digitize SOAP Note Assessments with SafetyCulture
SOAP note template PDFs offer practitioners a reliable way to maintain physical records of patient assessments. However, this traditional process can be significantly improved and streamlined by leveraging modern technology in daily operations. Digitizing SOAP note assessments provides numerous advantages, including:
Keep data in a centralized location so that records are stored in a single digital location, ensuring continuity of care even if a patient transitions between doctors
Ensure data security and compliance through access control and backup systems that make data accessible only to authorized personnel
Increase assessment efficiency with an intuitive digital interface and customizable templates that can be modified according to specific needs